How We Do It?
A 360-degree Prior Authorization Approach
Prior Authorization needs to be approached from an aspect of utilization management, specifically prospective utilization review, where an insurance payer looks at a number of factors such as medical necessity, prior treatment, clinical indications, and total cost of the therapy to determine whether a cost-savings could occur.
Utilization management is practised by both insurance payers and hospitals to rein in costs and reduce denials, but in the real world, PA is responsible for 92% of care delays, treatment abandonment, and 853 hours per year of wasted staff time.
Even with staff specifically designated to handle the bulk of the paperwork, insurance filing, and medical prior authorization processes, there is still a great deal to manage here. Not only do they (and you) have to ensure paperwork is filled out completely for every patient, but they also have to ensure each of the precertification is obtained in a timely manner, follow up on requests for more information from the physician, and deal with requested paper work or deal with denials. That’s not to mention the broader-scale tasks like keeping up with policy changes and staying up on training.
The paperwork and records are a necessary part of keeping a practice running smoothly. Of course, those little necessities here easily builds up into major hassle — one that affects everything from cash flow to patient experience — if the details are not handled appropriately.
The demands of the insurance prior authorization process can have a widespread impact on any medical practice, no matter how large or small. This is where Opry Medical Group steps in to help. Our insurance authorization process works as an extension of the client office every step of the way.
What is a Health Care Provider’s favorite pastime?
A 360-degree Prior Authorization Approach
We provide medical practices with knowledgeable precertification specialists to handle all the paperwork so your team can enjoy the freedom to focus on providing the best patient care.
We’ll take care of everything from initiating an insurance preauthorization request all the way through to appeal a denial.
Just as important, we keep our team in the know about updated processes and legal changes which affect health insurance so we can provide the best accuracy and efficiency with every precertification request.
Pre-authorizations will never be a Health Care Provider’s favorite pastime, but assembling as much information as possible before it’s needed can expedite the process and help reduce bundling denials related to authorizations. This does not only ensures timely patient care, but it also keeps medical practices in charge of the care they provide.
But the simplest method to beat the burden of getting prior authorizations is to modify with software and transmit approval requests digitally.

Time = Money
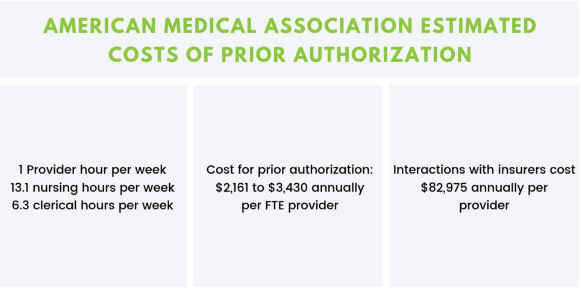
According to a study published on Health Affairs, when that time is calculated in dollars, median spending for a primary care practice to obtain PA is $47,707 per full-time physician––or $23 billion and $31 billion annually industry-wide.
According to the most recent study conducted by McKesson using the data from CAQH––An organization that monitors electronic adoption in healthcare; when faxes, phone calls, clinical time and other aspects are considered, labor costs to a doctor range from $35 to $100 per prior approval.
In 2016, 82% of pre-authorizations were done manually over the phone and fax, but during 2017, electronic adoption dropped from a high of 18% to just 8% today. During this same time period, the pre-authorization cost rose $1.8 billion, while the rate of administrative transactions to process them increased by 38%. but other groups like the AMA put the potential savings to physicians at two to three times that.
Do you know just how much pre-certifications are costing you each month? Connect with Opry today to get know more.
How Can We Help?
Take some time – Get in touch, and we’ll show you the difference Opry Medical Group can construct with your Revenue cycle. Fill out the form below to hear from a member of our team within 24 hours.
